Modernizing legacy systems in healthcare is necessary to take advantage of technological advancements and meet the changing needs of both patients and healthcare providers. Modernization makes it possible to incorporate innovative solutions like machine learning (ML) and artificial intelligence (AI), which improve patient outcomes, treatments, and diagnostic accuracy. Additionally, automating tasks, streamlining procedures, and enabling seamless data sharing among healthcare professionals, increases operational efficiency. Modernization also guarantees adherence to legal specifications, protecting patient information, and improving security protocols. According to Statista, The modernization of legacy systems in healthcare is expected to be driven mostly by enhancing security and efficiency, according to more than half of the surveyed businesses in 2023. Nearly half of the respondents also noted cost reduction, improved integration with contemporary technologies, and more agility and flexibility. This blog will cover the following topics: the importance of modernizing healthcare legacy systems; types of legacy healthcare systems; best practices for upgrading legacy medical systems; examples of healthcare legacy system modernization; and a set of challenges faced while using legacy systems. Let's explore further.
Types of Legacy Healthcare IT Systems
Legacy healthcare systems encompass a variety of healthcare software programs that were formerly utilized to assist various tasks within the healthcare industry. Below are the most known legacy healthcare IT systems:
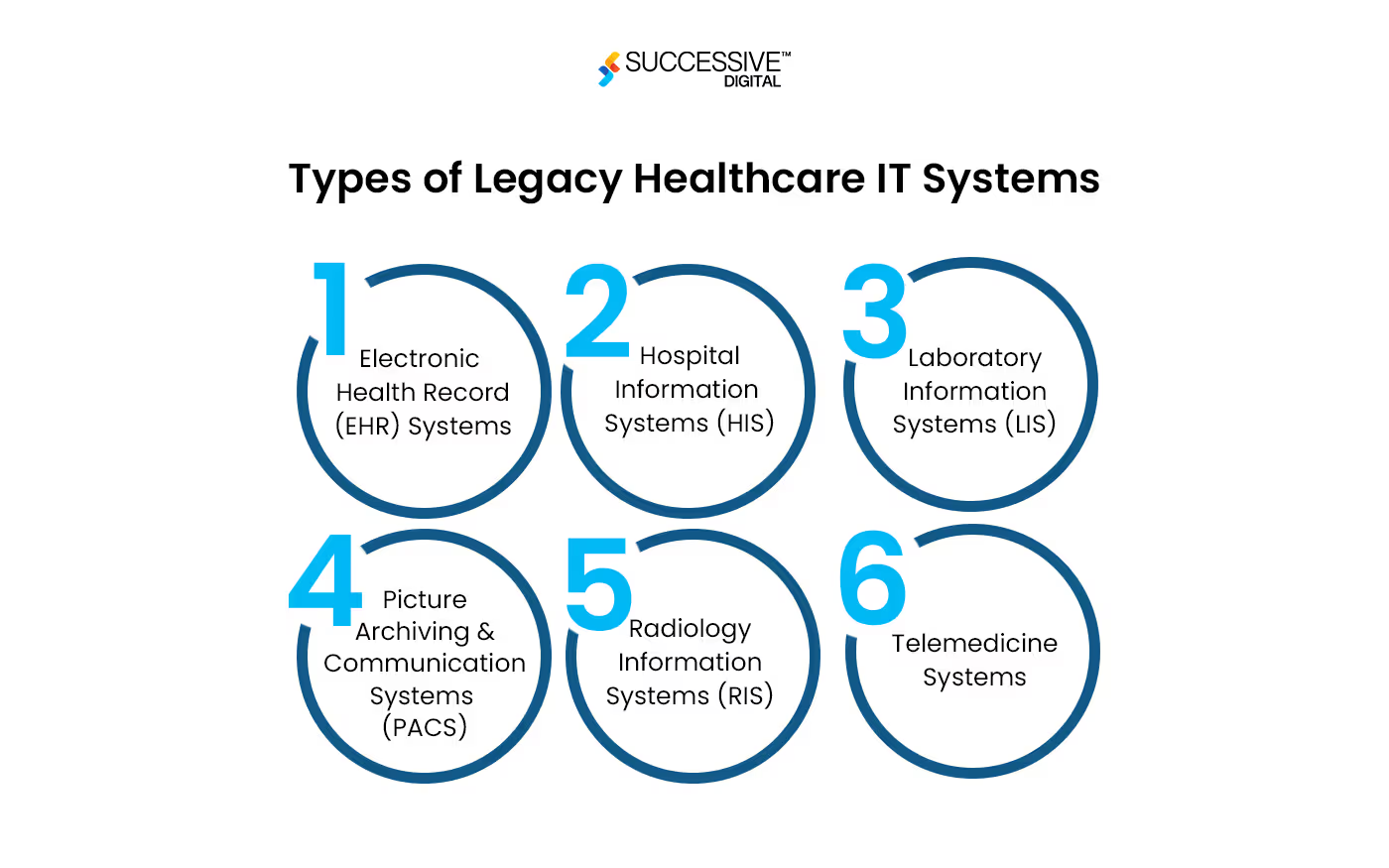
- Electronic Health Record (EHR) Systems
Early versions of EHR systems focused on keeping simple patient records. These systems eventually lack modern functionality, interoperability, and intuitive user interfaces. To embed advanced technologies it’s imperative to modernize legacy systems in healthcare.
- Hospital Information Systems (HIS)
Legacy HIS includes systems for managing various administrative, financial, and clinical aspects of hospital operations. Outdated HIS systems struggle with interoperability, real-time data access, and reporting capabilities.
- Laboratory Information Systems (LIS)
These systems manage laboratory data, such as workflow and test results. Legacy LIS faces data standards concerns and a lack of integration capabilities with new diagnostic technology.
- Picture Archiving and Communication Systems (PACS)
Legacy PACS primarily stores and retrieves medical images. Legacy systems have compatibility issues with advanced imaging technology and have low integration capabilities.
- Radiology Information Systems (RIS)
RIS oversees radiological imaging workflows, scheduling, and invoicing. Older RIS lack features such as automatic appointment scheduling and have integration concerns with newer RIS.
- Telemedicine Systems
Outdated telemedicine systems are among the legacy systems in the healthcare communications infrastructure. These healthcare systems must be improved to ensure secure communication and successful telehealth services.
- Claims Processing Systems
These systems coordinate billing and reimbursement between payers and healthcare providers. The complexities of modern billing regulations and regulatory changes present a significant challenge to outdated claims processing systems.
- Patient Engagement Systems
Modern solutions frequently have more user-friendly interfaces and functionalities than early patient engagement systems. To encourage patients to actively participate in their healthcare, these systems need to be updated.As the healthcare industry changes, these outdated legacy systems in healthcare must be updated to meet the needs of data security, interoperability, and technological advancements. Now let's understand the challenges of legacy medical systems.
Legacy Systems in Healthcare Challenges
Legacy systems have been utilized in all the industries. Every legacy system has its own set of challenges. We are here to understand the challenges of legacy systems in healthcare:
- Interoperability
The capacity of various software programs and healthcare systems to effortlessly share, interpret, and use data is known as interoperability. Integrating legacy systems with more modern technology and exchanging data across healthcare networks is challenging since these systems lack defined data formats and communication protocols. Inefficient medical delivery, duplicate data entry, and fragmented patient information result from this lack of interoperability. Interoperability issues also impede continuity and coordination of treatment, which affects patient outcomes and safety.
- Outdated User Interface
The user interfaces of legacy healthcare systems are often antiquated, complicated, and challenging to use. It's possible that these interfaces don't meet the changing requirements of healthcare professionals or comply with contemporary usability standards. With such issues, users can become frustrated, less productive, and resistant to embracing new technology. Outdated user interfaces are a potential factor in mistakes, data entry delays, and decreased patient safety. Healthcare companies must prioritize user-centered design concepts and make modern interface investments to improve usability and user pleasure to overcome this obstacle.
- Security Concerns
Healthcare organizations place a high priority on security since patient data is sensitive and cybersecurity attacks are becoming prevalent. In addition to frequently having weak security protections, legacy systems can be vulnerable to ransomware attacks, data breaches, and other security threats. These vulnerabilities could be caused by out-of-date software, weak encryption techniques, or insufficient access restrictions. The risk of security breaches is further increased by the possibility that patches or security updates are not regularly applied to legacy systems. Healthcare companies need to put strong cybersecurity measures in place, like encryption, multi-factor authentication, intrusion detection systems, and frequent security audits, to reduce security risks.
- Patient Engagement
To promote proactive healthcare management, patient satisfaction, and improved health outcomes, patient participation is essential. However, legacy systems do not have the patient engagement tools and capabilities necessary to enable patients to take an active role in their care. Patients find it more difficult to make educated decisions about their health. These systems only provide restricted access to medical records, communication channels, or instructional materials. Moreover, newer technologies make it easier to access healthcare services and information—like patient portals and mobile apps. Healthcare companies need to invest in upgrading their systems and promoting patient-centered treatment to improve patient engagement through interactive health management platforms, self-service tools, and tailored communication.
- Data Silos
Data silos develop when information is kept in different systems or divisions of a company, making it difficult to access, exchange, and analyze data across the enterprise. Legacy systems lead to data silos because of their fragmented architecture and lack of interaction with other systems. As a result, healthcare providers may struggle to gain a clear picture of patient data, resulting in incomplete or incorrect assessments of patient health status and treatment outcomes. Data silos also inhibit healthcare workers' collaboration and efforts to use data analytics for clinical decision support, population health management, and quality improvement activities. To solve data silos, healthcare companies must deploy data integration solutions, such as interoperable electronic health record (EHR) systems, data warehouses, or health information exchanges, that aggregate and standardize data from several sources. Furthermore, organizations should have data governance rules and procedures to ensure data quality, security, and compliance throughout the organization.These are a set of challenges that are frequently faced in legacy systems in healthcare. Let’s understand how you can modernize your legacy medical systems.
How to Modernize Legacy Medical Systems?
Modernizing legacy data systems in the healthcare industry entails taking calculated steps to improve and upgrade out-of-date healthcare systems while making sure they comply with emerging technologies and industry standards. The following are some of the most important actions in updating legacy healthcare systems:
- Evaluation and Record-Keeping
Conduct a thorough analysis of the existing legacy systems, taking note of their dependability, functionality, and data formats. Record the precise integration specifications and objectives, keeping security and scalability in mind.
- Specify Integration Goals
Clearly define your integration goals, such as improved data flow, increased functionality, or compliance with new technology. Align these with the goals of your healthcare company to ensure that the integration strategy benefits the broader business.
- Choose an Integration Method
Choose an integration strategy based on the evaluated requirements and present infrastructure, such as data migration, APIs, middleware, or a combination of these alternatives. Consider the chosen method's long-term viability and scalability to ensure that it meets the organization's changing needs.
- Integration of Middleware
When using middleware, make sure it can ease communication between modern applications and legacy systems. Configure middleware to provide a smooth data transfer and system interoperability.
- API Integration
When using APIs, design or select ones that operate with both modern and legacy applications. To protect data during integration, make sure the appropriate authorization and authentication mechanisms are in place.
- Data Migration
Plan and execute data transfer from existing legacy systems in healthcare infrastructure to the new environment. Check the data's consistency and accuracy after migration.
- Testing
Thoroughly test the interconnected systems to ensure that they function as intended. Conduct user acceptance, integration, and unit testing to identify and correct faults and malfunctions.
- Implementation
To minimize disruptions to ordinary operations, choose a phased and progressive approach to integration. Monitor the integration process and address any issues that arise.
- Monitoring and Optimization
Use monitoring tools to track user feedback and system performance. Continue to improve the linked systems to meet evolving business needs and user experiences.By following these steps you can effectively plan your modernization strategy and embed advanced technologies within your existing ecosystem. But when you need expert support, we are here to help.
How Can Successive Digital Help You Modernize Your Healthcare Legacy Systems?
Healthcare applications have the potential to transform patient care, but their success will be determined by how successfully they interact with the legacy systems that underpin most of the healthcare sector. Despite the hurdles, modernizing outdated healthcare IT systems provides numerous benefits. As a result, the future of healthcare requires the cohabitation of legacy systems and technologies with the potential to improve patient outcomes and overall system efficacy. Here’s a story of how we helped one of our client in modernizing their legacy system in healthcare. Successive collaborated with a MedTech healthcare provider, to address key challenges in redefining the at-home screening experience through their App. The application initially faced issues with non-standard coding practices, inadequate adherence to medical regulations for patient data security, and inefficiencies in supporting new client onboarding and cross-functional team usage. Successive swiftly modernized legacy application by migrating it to AWS cloud infrastructure, enabling seamless day-to-day operations and remote at-home medical screening, especially vital during the COVID-19 pandemic. Their solutions included transforming the single-instance application into a multi-tier architecture, implementing robust security and compliance measures to support global expansion, and setting up scalable and fault-tolerant cloud infrastructure. Additionally, Successive integrated the ADP marketplace as a new service, enhancing HEDIS quality. This case study exemplifies Successive's expertise in delivering tailored healthcare solutions, emphasizing their proficiency in addressing complex challenges and driving innovation in the healthcare industry.Successive Digital's legacy healthcare solutions are focused on supporting the seamless integration of advanced technologies with legacy systems, which continue to be the foundation of the healthcare industry.
Conclusion
When it comes to growing or gaining a competitive edge, an organization's system or software can make all the difference in the modern digital age. This indicates that it is imperative to consider the software's ability to adapt to changing business requirements. This is where a carefully considered modernization approach for legacy systems is beneficial.IDC predicts that by 2024, the majority of legacy programs will probably be modernized. Furthermore, 65 percent of these applications will probably make use of cloud services to update outdated code or enhance overall functionality. Updating legacy systems will certainly be a popular trend in 2024. Are you also struggling with outdated systems, we are here to help! We can transform your legacy systems and turn your imagination into reality. Contact us Today!
.avif)





.jpg)




.jpg)









